Workers’ Compensation Claims Management
Turn your revenue cycle challenges into financial opportunities
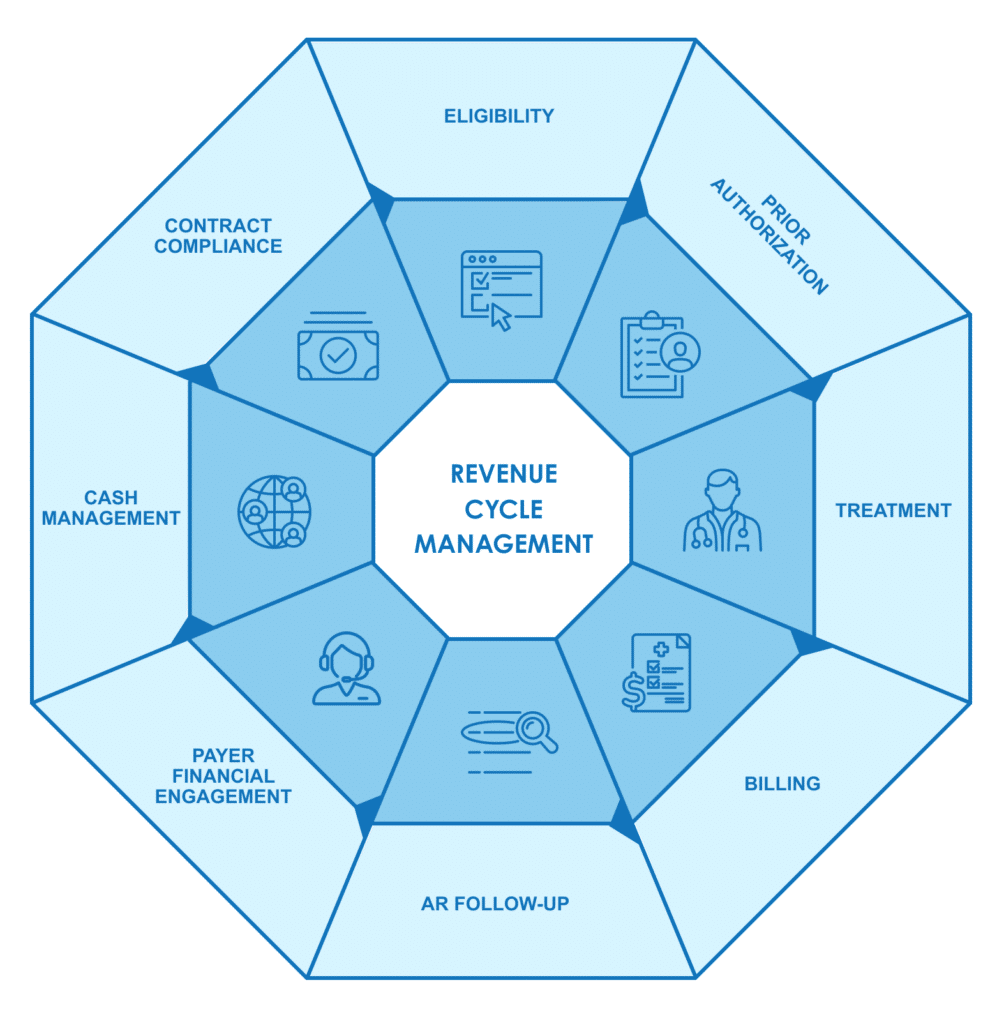
Timely and accurate Workers’ Compensation payments are essential for healthcare providers, yet delays and denials are common due to administrative bottlenecks, eligibility issues, a lack of authorization, and missed deadlines. With strict state, federal, and payer timely filing limits ranging from 60 days to a year—and appeal periods as short as 30 days—proactive revenue cycle management of your Workers’ Compensation claims is critical.
At Unified Health Services, we specialize in optimizing Workers’ Compensation claims, ensuring faster reimbursements, fewer denials, and full compliance. Backed by 25+ years of experience and more than $8 billion in claims billed, our solutions improve your financial outcomes.

2%
Denial Rate
$4,500
Saved Per Claim
8
Days for Prior Authorization
>75%
EDI Rate
>95%
First Pass Rate
Our solutions
Day 1 – RCM Services
From the moment a patient is registered, we manage every step—verifying the employer, jurisdiction, pay-to address, eligibility, billing, accounts receivable follow-up, denial management, appeals, and payment processing—all while eliminating compliance errors to streamline operations and accelerate your payments.

What Sets Our Solution Apart
Our offering is the only end-to-end solution in Workers’ Compensation revenue cycle management.
“Unified Health Services’ expertise has transformed our Workers’ Compensation billing, significantly improving our financial performance.”
– RCM Administrator
Got a backlog? Stop chasing payments
Are you sitting on a backlog of delays, denials, and unpaid Workers’ Compensation claims? Older Workers’ Compensation claims (30+ days) can negatively impact your cash flow. Our Day 30+ Old AR RCM Services are designed to efficiently recover these aged claims, capturing lost revenue and resolving backlogs that keep your team from focusing on current claims.
This is the perfect way to get your foot in the door. Let us handle the hassle of claims so you can focus on what you do best.
Start Recovering Lost Revenue Today

How we help
Hospitals
Hospitals manage a diverse payer mix where 90% of their business is with 10 payers or less — 50% are through government programs such as Medicare/Medicaid, 40% commercial insurance, and the remaining 10% can easily exceed 300 payers.
Our solutions streamline payer management, improve billing, centralize verification, and optimize high-value claims—helping you maximize revenue and efficiency.
Ambulatory surgery centers (ASC)
Ambulatory Surgery Centers (ASCs) operate under diverse ownership models and face complex multi-state insurance challenges.
With a “trust but verify” approach to prior eligibility, benefit verification, and prior authorizations, ASCs benefit from verification services that verify payment before a claim is submitted which reduces denials and rework.
Health systems
Health systems revenue cycle and finance executives are focused on improving operational efficiency, reducing the cost of care, to improve the both the patient experience, but also improved financial outcomes.
Our solutions streamline RCM processes while delivering measurable financial improvements—keeping operations efficient and finance teams confident in the results.